Affiliate Disclaimer:
Some of the links on this website are affiliate links, which means that if you click on a link and make a purchase, we may earn a commission at no extra cost to you. This helps support the website and allows us to continue creating content. We only recommend products or services we personally use or genuinely believe will add value to our readers.
Periodontitis is a serious gum disease affecting millions worldwide. As a dental professional, I’ve seen firsthand the devastating effects of untreated periodontitis, from painful gum inflammation to tooth loss.
But I’ve also seen remarkable transformations in patients who receive proper treatment.
In this comprehensive guide, I’ll walk you through the latest approaches to treating periodontitis and restoring oral health.
Understanding Periodontitis
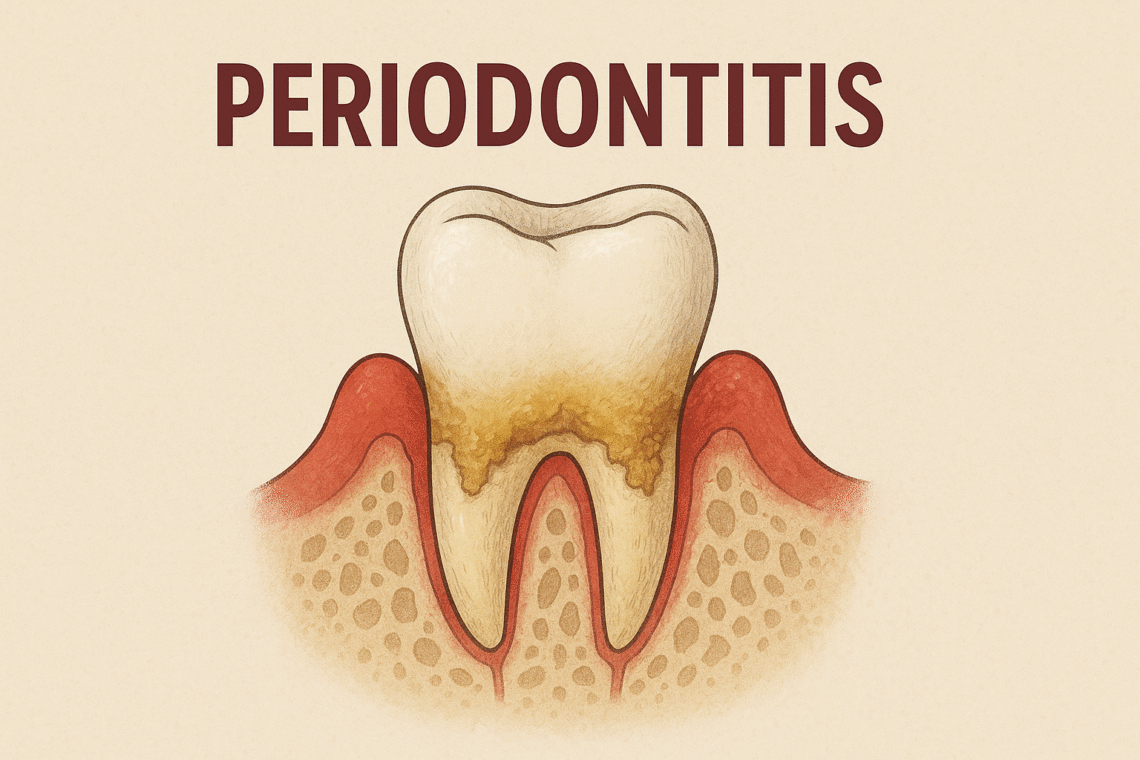
Periodontitis is an advanced stage of gum disease characterized by inflammation of the gums and supporting structures of the teeth. It begins with the buildup of bacterial plaque and tartar, leading to the formation of periodontal pockets, bone loss, and potential tooth loss if left untreated.
Several factors contribute to the development of periodontitis:
Poor oral hygiene
Smoking
Genetic predisposition
Certain systemic diseases (e.g., diabetes)
Hormonal changes
Medications that reduce saliva flow
Nutritional deficiencies
Recognizing periodontitis early is crucial for effective treatment. Common signs include:
Red, swollen, or tender gums
Bleeding while brushing or flossing
Receding gums
Loose teeth
Persistent bad breath
Changes in bite or tooth alignment
Non-Surgical Treatments
Scaling and Root Planing (SRP)
SRP remains the standard approach for managing periodontitis. The procedure clears plaque and tartar from areas above and beneath the gumline and smooths root surfaces, supporting tissue healing and gum reattachment.
During SRP, I use specialized instruments to thoroughly clean the teeth and root surfaces. The process can take multiple appointments, depending on the severity of the condition.
Many patients report significant improvement in gum health and reduced inflammation after SRP.
Antimicrobial Therapy
Antimicrobial treatments often complement SRP to control bacterial infection. These may include:
Local antibiotics: Applied directly to affected areas
Systemic antibiotics: Taken orally to address widespread infection
Antimicrobial mouth rinses: Used at home to support ongoing treatment
One exciting advancement in this area is the development of controlled-release local antibiotic delivery systems. These allow for targeted treatment of specific problem areas, minimizing side effects and maximizing effectiveness.
Oral Hygiene Education
Successful periodontitis treatment relies heavily on proper at-home care. I work closely with patients to improve their oral hygiene routines, covering:
Proper brushing techniques
Effective flossing methods
Use of interdental cleaning tools (e.g., water flossers, interdental brushes)
Importance of regular dental check-ups
Many patients are surprised to learn they’ve been brushing or flossing incorrectly for years. Small adjustments to technique can make a significant difference in managing periodontitis.
Surgical Interventions
For advanced cases of periodontitis, surgical treatments may be necessary to restore oral health.
Flap Surgery
Flap surgery involves lifting back the gums to remove tartar deposits and reduce pocket depth. This procedure allows for thorough cleaning of the root surfaces and reshaping of damaged bone.
While the idea of gum surgery might sound intimidating, many patients report that the procedure is less uncomfortable than they anticipated. The results can be dramatic, with significant improvements in gum health and tooth stability.
Bone and Tissue Grafts
In cases where periodontitis has caused significant bone or tissue loss, grafting procedures can help regenerate these structures. There are several types of grafts:
Bone grafts: Using natural or synthetic bone to promote new bone growth
Soft tissue grafts: Often using tissue from the roof of the mouth to cover exposed root surfaces
Guided tissue regeneration: Using a special membrane to encourage the regrowth of specific tissues
These regenerative techniques can help save teeth that might otherwise be lost to advanced periodontitis.
Emerging Technologies in Periodontitis Treatment
The field of periodontal care is constantly evolving, with new technologies offering promising results.
Laser Therapy
Laser treatments for periodontitis are gaining popularity because of their precision and ability to promote healing. Different types of lasers can:
Remove diseased tissue
Kill bacteria in periodontal pockets
Stimulate gum reattachment
Many patients appreciate laser therapy for its minimally invasive nature and reduced post-treatment discomfort.
Photodynamic Therapy
This innovative treatment uses light-activated antimicrobial agents to target and destroy bacteria in periodontal pockets. The process involves:
Applying a photosensitizing agent to the affected areas
Illuminating the area with a specific wavelength of light
The light activates the agent, creating oxygen molecules that kill bacteria
Photodynamic therapy shows promise in treating areas that are difficult to reach with traditional methods.
Platelet-Rich Plasma (PRP) Therapy
PRP therapy uses growth factors from a patient’s own blood to accelerate healing and tissue regeneration. The process involves:
Drawing a small amount of the patient’s blood
Processing it to concentrate the platelets
Applying the platelet-rich plasma to the treatment site
Early studies show promising results in promoting faster healing and improved outcomes in periodontal procedures.
Stem Cell Therapy
While still in experimental stages, stem cell therapy for periodontal regeneration holds exciting potential. Researchers are exploring ways to use stem cells to regrow lost periodontal tissues, potentially altering how we treat advanced periodontitis.
The Periodontal-Systemic Health Connection
Treating periodontitis extends beyond saving teeth. A growing body of research reveals a bidirectional relationship between periodontal health and overall systemic health.
By addressing gum disease, we may positively impact:
Cardiovascular health: Reducing inflammation may lower the risk of heart disease
Diabetes management: Improved periodontal health can lead to better blood sugar control
Respiratory health: Decreasing oral bacteria may reduce the risk of respiratory infections
Cognitive function: Some studies suggest a link between gum disease and cognitive decline
This connection underscores the importance of comprehensive periodontal care as part of overall health management.
Long-Term Maintenance and Lifestyle Changes
Successful periodontitis treatment needs ongoing care and lifestyle adjustments.
Regular Maintenance Appointments
I typically recommend periodontal maintenance appointments every 3-4 months. These visits allow for:
Professional cleaning to remove any new plaque and tartar buildup
Monitoring of gum health and pocket depths
Early intervention if signs of recurrence appear
Smoking Cessation
Quitting smoking significantly improves treatment outcomes and reduces the risk of periodontitis recurrence. I work with patients to develop smoking cessation strategies or refer them to specialized programs.
Managing Systemic Conditions
For patients with conditions like diabetes, effective management of their systemic health can have a positive impact on periodontal health. I often collaborate with patients’ primary care physicians to confirm comprehensive care.
Stress Management
Chronic stress can negatively affect immune function and periodontal health. I talk about stress management techniques with patients, such as:
Regular exercise
Meditation or mindfulness practices
Adequate sleep
Seeking professional help if needed
Nutritional Support
A balanced diet rich in vitamins and minerals supports periodontal health. I advise patients on foods that promote gum health, such as:
Vitamin C-rich fruits and vegetables
Omega-3 fatty acids found in fish and nuts
Calcium and vitamin D for bone health
The Future of Periodontitis Treatment
As research continues, we’re likely to see even more advanced treatments for periodontitis. Some areas of ongoing investigation include:
Personalized treatment based on genetic markers
Advanced biomaterials for tissue regeneration
Targeted immunomodulation therapies
Probiotic treatments to promote useful oral bacteria
These developments hold the promise of more effective, less invasive treatments for periodontitis in the future.
Key Takeaways
Periodontitis is a severe form of gum disease requiring comprehensive treatment.
Non-surgical therapies like scaling and root planing form the foundation of treatment.
Advanced cases may require surgical interventions and regenerative procedures.
Emerging technologies such as laser therapy and PRP show promise in periodontal treatment.
Treating periodontitis can have positive effects on overall health.
Long-term success depends on consistent maintenance and lifestyle changes.
With proper treatment and care, achieving lasting periodontal health is possible.
People Also Asked
What are the early signs of periodontitis?
Early signs of periodontitis include red, swollen, or bleeding gums, persistent bad breath, and gum recession. If you notice these symptoms, it’s crucial to see a dentist promptly for evaluation and treatment.
How long does it take to treat periodontitis?
The duration of periodontitis treatment varies depending on the severity of the condition. Initial treatment typically takes several weeks to months, with ongoing maintenance required indefinitely to prevent recurrence.
Can periodontitis be reversed?
While early-stage periodontitis can often be reversed with proper treatment and care, advanced cases may only be managed rather than fully reversed. Early intervention is key to achieving the best possible outcomes.
Is periodontitis treatment painful?
Most periodontitis treatments cause minimal discomfort. Local anesthesia is used for procedures like scaling and root planing.
Post-treatment sensitivity is common but typically decides within a few days.
How often should I have periodontal maintenance after treatment?
After initial treatment, most patients require periodontal maintenance appointments every 3-4 months. Your dentist will recommend a schedule based on your person needs and response to treatment.
Can periodontitis affect overall health?
Yes, periodontitis has been linked to various systemic health issues, including heart disease, diabetes, and respiratory problems. Treating periodontitis may have positive effects on overall health.
Are there natural remedies for periodontitis?
While professional treatment is essential for managing periodontitis, some natural remedies may support gum health. These include oil pulling, green tea consumption, and using aloe vera gel.
However, these should not replace professional care.
How does smoking affect periodontitis treatment?
Smoking significantly reduces the effectiveness of periodontitis treatment and increases the risk of recurrence. Quitting smoking greatly improves treatment outcomes and overall oral health.
Can stress cause periodontitis to worsen?
Chronic stress can negatively impact immune function and periodontal health. Managing stress through relaxation techniques, exercise, and adequate sleep can support periodontal treatment outcomes.
Is laser treatment for periodontitis effective?
Laser therapy shows promising results in periodontitis treatment, offering precision and promoting healing. However, it’s typically used in conjunction with traditional treatments rather than as a standalone solution.